Subarachnoid hemorrhage
| Subarachnoid hemorrhage | |
|---|---|
| Classification and external resources | |
 CT scan of the brain showing subarachnoid hemorrhage as a white area in the center and stretching into the sulci to either side (marked by the arrow) |
|
| ICD-10 | I60., P10.3, S06.6 |
| ICD-9 | 430, 852.0-852.1 |
| OMIM | 105800 |
| DiseasesDB | 12602 |
| MedlinePlus | 000701 |
| eMedicine | med/2883 neuro/357 emerg/559 |
| MeSH | D013345 |
A subarachnoid hemorrhage (SAH, pronounced /ˌsʌbəˈræknɔɪd ˈhɛm(ə)rɪdʒ/, or subarachnoid haemorrhage in British English) is bleeding into the subarachnoid space—the area between the arachnoid membrane and the pia mater surrounding the brain. This may occur spontaneously, usually from a ruptured cerebral aneurysm, or may result from head injury.
Symptoms of SAH include a severe headache with a rapid onset ("thunderclap headache"), vomiting, confusion or a lowered level of consciousness, and sometimes seizures.[1] The diagnosis is generally confirmed with a CT scan of the head, or occasionally by lumbar puncture. Treatment is by prompt neurosurgery or radiologically guided interventions with medications and other treatments to help prevent recurrence of the bleeding and complications. Surgery for aneurysms was introduced in the 1930s, but since the 1990s many aneurysms are treated by a less invasive procedure called "coiling", which is carried out by instrumentation through large blood vessels.[1]
SAH is a form of stroke and comprises 1–7% of all strokes.[2] It is a medical emergency and can lead to death or severe disability—even when recognized and treated at an early stage. Up to half of all cases of SAH are fatal and 10–15% die before reaching a hospital,[1] and those who survive often have neurological or cognitive impairment.[3]
Contents |
Signs and symptoms
The classic symptom of subarachnoid hemorrhage is thunderclap headache (a headache described as "like being kicked in the head",[4] or the "worst ever", developing over seconds to minutes). This headache often pulsates towards the occiput (the back of the head).[5] About one-third of sufferers have no symptoms apart from the characteristic headache, and about one in ten people who seek medical care with this symptom are later diagnosed with a subarachnoid hemorrhage.[1] Vomiting may be present, and 1 in 14 have seizures.[1] Confusion, decreased level of consciousness or coma may be present, as may neck stiffness and other signs of meningism.[1] Neck stiffness usually presents six hours after initial onset of SAH.[6] Isolated dilation of a pupil and loss of the pupillary light reflex may reflect brain herniation as a result of rising intracranial pressure (pressure inside the skull).[1] Intraocular hemorrhage (bleeding into the eyeball) may occur in response to the raised pressure: subhyaloid hemorrhage (bleeding under the hyaloid membrane, which envelops the vitreous body of the eye) and vitreous hemorrhage may be visible on fundoscopy. This is known as Terson syndrome (occurring in 3–13% of cases) and is more common in more severe SAH.[7]
Oculomotor nerve abnormalities (affected eye looking downward and outward and inability to lift the eyelid on the same side) or palsy (loss of feeling) may indicate bleeding from the posterior communicating artery.[1][5] Seizures are more common if the hemorrhage is from an aneurysm; it is otherwise difficult to predict the site and origin of the hemorrhage from the symptoms.[1] SAH in a person known to have fits is often diagnostic of an arteriovenous malformation.[5]
As a result of the bleeding, the body releases large amounts of adrenaline and similar hormones. This leads to a sharp increase in the blood pressure; the heart comes under substantial strain, and neurogenic pulmonary edema (accumulation of fluid in the lungs), cardiac arrhythmias (irregularities in the heart rate and rhythm), electrocardiographic changes (in 27% of cases)[8] and cardiac arrest (in 3% of cases) may occur rapidly after the onset of hemorrhage.[1][9]
Subarachnoid hemorrhage may also occur in people who have suffered a head injury. Symptoms may include headache, decreased level of consciousness and hemiparesis (weakness of one side of the body). SAH is a frequent occurrence in traumatic brain injury, and carries a poor prognosis if it is associated with deterioration in the level of consciousness.[10]
Causes
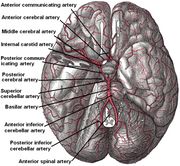
In 85% of cases of spontaneous SAH, the cause is rupture of a cerebral aneurysm—a weakness in the wall of one of the arteries in the brain that becomes enlarged. They tend to be located in the circle of Willis and its branches. While most cases of SAH are due to bleeding from small aneurysms, larger aneurysms (which are less common) are more likely to rupture.[1]
In 15–20% of cases of spontaneous SAH, no aneurysm is detected on the first angiogram.[11] About half of these are attributed to non-aneurysmal perimesencephalic hemorrhage, in which the blood is limited to the subarachnoid spaces around the midbrain (i.e. mesencephalon). In these, the origin of the blood is uncertain.[1] The remainder are due to other disorders affecting the blood vessels (such as arteriovenous malformations), disorders of the blood vessels in the spinal cord, and bleeding into various tumors.[1] Cocaine abuse and sickle cell anemia (usually in children) and, rarely, anticoagulant therapy, problems with blood clotting and pituitary apoplexy can also result in SAH.[6][11]
Subarachnoid blood can be detected on CT scanning in as many as 60% of people with traumatic brain injury.[12] Traumatic SAH (tSAH) usually occurs near the site of a skull fracture or intracerebral contusion.[11] It usually happens in the setting of other forms of traumatic brain injury and has been linked with a poorer prognosis. It is unclear, however, if this is a direct result of the SAH or whether the presence of subarachnoid blood is simply an indicator of severity of the head injury and the prognosis is determined by other associated mechanisms.[12]
Diagnosis

Imaging
The initial steps for evaluating a person with a suspected subarachnoid hemorrhage are obtaining a medical history and performing a physical examination; these are aimed at determining whether the symptoms are due to SAH or to another cause. The diagnosis cannot, however, be made on clinical grounds alone; therefore medical imaging is generally required to confirm or exclude bleeding. The modality of choice is computed tomography (CT scan) of the brain. This has a high sensitivity and will correctly identify over 95% of cases—especially on the first day after the onset of bleeding. Magnetic resonance imaging (MRI) may be more sensitive than CT after several days.[1]
Lumbar puncture
Lumbar puncture, in which cerebrospinal fluid (CSF) is removed with a needle from the lumbar sac, will show evidence of hemorrhage in 3% of people in whom CT was found normal; lumbar puncture is therefore regarded as mandatory in people with suspected SAH if imaging is negative.[1] At least three tubes of CSF are collected.[6] If an elevated number of red blood cells is present equally in all bottles, this indicates a subarachnoid hemorrhage. If the number of cells decreases per bottle, it is more likely that it is due to damage to a small blood vessel during the procedure (known as a "traumatic tap").[3] The CSF sample is also examined for xanthochromia—the yellow appearance of centrifugated fluid. More sensitive is spectrophotometry (measuring the absorption of particular wavelengths of light) for detection of bilirubin, a breakdown product of hemoglobin from red blood cells.[1][13] Xanthochromia and spectrophotometry remain reliable ways to detect SAH several days after the onset of headache.[13] An interval of at least 12 hours between the onset of the headache and lumbar puncture is required, as it takes several hours for the hemoglobin from the red blood cells to be metabolized into bilirubin.[1][13]
As only 10% of people admitted to the emergency department with a thunderclap headache are suffering from an SAH, other possible causes are usually considered simultaneously, such as meningitis, migraine, and cerebral venous sinus thrombosis.[4] Intracerebral hemorrhage, in which bleeding occurs within the brain itself, is twice as common as SAH and is often misdiagnosed as the latter.[14] It is not unusual for SAH to be initially misdiagnosed as a migraine or tension headache, which can lead to a delay in obtaining a CT scan. In a 2004 study, this occurred in 12% of all cases and was more likely in people who had smaller hemorrhages and no impairment in their mental status. The delay in diagnosis led to a worse outcome.[15] In some people, the headache resolves by itself, and no other symptoms are present. This type of headache is referred to as "sentinel headache", because it is presumed to result from a small leak (a "warning leak") from an aneurysm. A sentinel headache still warrants investigations with CT scan and lumbar puncture, as further bleeding may occur in the subsequent three weeks.[3]
Angiography
After a subarachnoid hemorrhage is confirmed, its origin needs to be determined. If the bleeding is likely to have originated from an aneurysm (as determined by the CT scan appearance), the choice is between cerebral angiography (injecting radiocontrast through a catheter to the brain arteries) and CT angiography (visualizing blood vessels with radiocontrast on a CT scan) to identify aneurysms. Catheter angiography also offers the possibility of coiling an aneurysm (see below).[1][3]
ECG
Electrocardiographic changes are relatively common in subarachnoid hemorrhage, occurring in 40–70% of cases. They may include QT prolongation, Q waves, cardiac dysrhythmias and ST elevation that mimics a heart attack.[16]
Classification
There are several grading scales available for SAH. The Glasgow Coma Scale is ubiquitously used for assessing consciousness. Three specialized scores are used to evaluate SAH; in each, a higher number is associated with a worse outcome.[17] These scales have been derived by retrospectively matching characteristics of patients with their outcomes.
The first scale of severity was described by Hunt and Hess in 1968:[18]
| Grade | Signs and symptoms | Survival |
|---|---|---|
| 1 | Asymptomatic or minimal headache and slight neck stiffness | 70% |
| 2 | Moderate to severe headache; neck stiffness; no neurologic deficit except cranial nerve palsy | 60% |
| 3 | Drowsy; minimal neurologic deficit | 50% |
| 4 | Stuporous; moderate to severe hemiparesis; possibly early decerebrate rigidity and vegetative disturbances | 20% |
| 5 | Deep coma; decerebrate rigidity; moribund | 10% |
The Fisher Grade classifies the appearance of subarachnoid hemorrhage on CT scan.[19] This scale has been modified by Claassen and coworkers, reflecting the additive risk from SAH size and accompanying intraventricular hemorrhage.[20]
| Grade | Appearance of hemorrhage |
|---|---|
| 1 | None evident |
| 2 | Less than 1 mm thick |
| 3 | More than 1 mm thick |
| 4 | Any thickness with intraventricular hemorrhage or parenchymal extension |
The World Federation of Neurosurgeons (WFNS) classification uses Glasgow coma score (GCS) and focal neurological deficit to gauge severity of symptoms.[21]
| Grade | GCS | Focal neurological deficit |
|---|---|---|
| 1 | 15 | Absent |
| 2 | 13–14 | Absent |
| 3 | 13–14 | Present |
| 4 | 7–12 | Present or absent |
| 5 | <7 | Present or absent |
A comprehensive classification scheme has been suggested by Ogilvy and Carter to predict outcome and gauge therapy.[22] The system consists of five grades and it assigns one point for the presence or absence of each of five factors: age greater than 50; Hunt and Hess grade 4 or 5; Fisher scale 3 or 4; aneurysm size greater than 10 mm; and posterior circulation aneurysm 25 mm or more.[22]
Screening and prevention
Screening for aneurysms is not performed on a population level; because they are relatively rare, it would not be cost-effective. If someone has two or more first-degree relatives who have suffered an aneurysmal subarachnoid hemorrhage, screening may be worthwhile.[1][23]
Autosomal dominant polycystic kidney disease (ADPKD), a hereditary kidney condition, is known to be associated with cerebral aneurysms in 8% of cases, but most such aneurysms are small and therefore unlikely to rupture. As a result, screening is only recommended in families with ADPKD where one family member has suffered a ruptured aneurysm.[24]
An aneurysm may be detected incidentally on brain imaging; this presents a conundrum, as all treatments for cerebral aneurysms are associated with potential complications. The International Study of Unruptured Intracranial Aneurysms (ISUIA) provided prognostic data both in people who had previously suffered a subarachnoid hemorrhage and people who had aneurysms detected by other means. Those who had previously suffered SAH were more likely to bleed from other aneurysms. In contrast, those who had never bled and had small aneurysms (smaller than 10 mm) were very unlikely to suffer SAH and were likely to sustain harm from attempts to repair these aneurysms.[25] On the basis of the ISUIA and other studies, it is now recommended that people are only considered for preventative treatment if they have a reasonable life expectancy and have aneurysms that are highly likely to rupture.[23]
Treatment
Management involves general measures to stabilize the patient while also using specific investigations and treatments. These include the prevention of rebleeding by obliterating the bleeding source, prevention of a phenomenon known as vasospasm, and prevention and treatment of complications.[1]
General measures
Stabilizing the patient is the first priority. Those with a depressed level of consciousness may need to be intubated and mechanically ventilated. Blood pressure, pulse, respiratory rate and Glasgow Coma Scale are monitored frequently. Once the diagnosis is confirmed, admission to an intensive care unit may be preferable, especially since 15% may have further bleeding soon after admission. Nutrition is an early priority, with oral or nasogastric tube feeding being preferable over parenteral routes. Analgesia (pain control) is generally restricted to less sedating agents such as codeine, as sedation may impact on the mental status and thus interfere with the ability to monitor the level of consciousness. Deep vein thrombosis is prevented with compression stockings, intermittent pneumatic compression of the calves or both.[1] A bladder catheter is usually inserted to monitor fluid balance. Benzodiazepines may be administered to help relieve distress.[6] Antiemetic drugs should be given to awake persons.[5]
Prevention of rebleeding
People whose CT scan shows a large hematoma, depressed level of consciousness or focal neurologic symptoms may benefit from urgent surgical removal of the blood or occlusion of the bleeding site. The remainder are stabilized more extensively and undergo an transfemoral angiogram or CT angiogram later. It is hard to predict who will suffer a rebleed, yet it may happen at any time and carries a dismal prognosis. After the first 24 hours have passed, rebleeding risk remains around 40% over the subsequent four weeks, suggesting that interventions should be aimed at reducing this risk as soon as possible.[1]
If a cerebral aneurysm is identified on angiography, two measures are available to reduce the risk of further bleeding from the same aneurysm: clipping[26] and coiling.[27] Clipping requires a craniotomy (opening of the skull) to locate the aneurysm, followed by the placement of clips around the neck of the aneurysm. Coiling is performed through the large blood vessels (endovascularly): a catheter is inserted into the femoral artery in the groin and advanced through the aorta to the arteries (both carotid arteries and both vertebral arteries) that supply the brain. When the aneurysm has been located, platinum coils are deployed that cause a blood clot to form in the aneurysm, obliterating it. The decision as to which treatment is undertaken is typically made by a multidisciplinary team consisting of a neurosurgeon, neuroradiologist and often other health professionals.[1]
Generally, the decision between clipping and coiling is made on the basis of the location of the aneurysm, its size and the condition of the patient. Aneurysms of the middle cerebral artery and its related vessels are hard to reach with angiography and tend to be amenable to clipping. Those of the basilar artery and posterior cerebral artery are hard to reach surgically and are more accessible for endovascular management.[28] These approaches are based on general experience, and the only randomized controlled trial directly comparing the different modalities was performed in relatively well patients with small (less than 10 mm) aneurysms of the anterior cerebral artery and anterior communicating artery (together the "anterior circulation"), who constitute about 20% of all patients with aneurysmal SAH.[28][29] This trial, the International Subarachnoid Aneurysm Trial (ISAT), showed that in this group the likelihood of death or being dependent on others for activities of daily living was reduced (7.4% absolute risk reduction, 23.5% relative risk reduction) if endovascular coiling was used as opposed to surgery.[28] The main drawback of coiling is the possibility that the aneurysm will recur; this risk is extremely small in the surgical approach. In ISAT, 8.3% needed further treatment in the longer term. Hence, people who have undergone coiling are typically followed up for many years afterwards with angiography or other measures to ensure recurrence of aneurysms is identified early.[30] Other trials have also found a higher rate of recurrence necessitating further treatments.[31][32]
Vasospasm
Vasospasm, in which the blood vessels constrict and thus restrict blood flow, is a serious complication of SAH. It can cause ischemic brain injury (referred to as "delayed ischemia") and permanent brain damage due to lack of oxygen in parts of the brain. It can be fatal if severe. Delayed ischemia is characterized by new neurological symptoms, and can be confirmed by transcranial doppler or cerebral angiography. About one third of all people admitted with subarachnoid hemorrhage will have delayed ischemia, and half of those suffer permanent damage as a result.[33] It is possible to screen for the development of vasospasm with transcranial doppler every 24–48 hours. A blood flow velocity of more than 120 centimeters per second is suggestive of vasospasm.[3]
The use of calcium channel blockers, thought to be able to prevent the spasm of blood vessels by preventing calcium from entering smooth muscle cells, has been proposed for the prevention of vasospasm.[12] The oral calcium channel blocker nimodipine improves outcome if administered between the fourth and twenty-first day after the hemorrhage, even if it does not significantly reduce the amount of vasospasm detected on angiography.[34] In traumatic subarachnoid hemorrhage, nimodipine does not affect long-term outcome, and is not recommended.[35] Other calcium channel blockers and magnesium sulfate have been studied, but are not presently recommended; neither is there any evidence that shows benefit if nimodipine is given intravenously.[33]
A protocol referred to as "triple H" is often used as a measure to treat vasospasm when it causes symptoms; this is the use of intravenous fluids to achieve a state of hypertension (high blood pressure), hypervolemia (excess fluid in the circulation) and hemodilution (mild dilution of the blood).[36] Evidence for this approach is inconclusive; no randomized controlled trials have been undertaken to demonstrate its benefits.[37]
If the symptoms of delayed ischemia do not improve with medical treatment, angiography may be attempted to identify the sites of vasospasms and administer vasodilator medication (drugs that relax the blood vessel wall) directly into the artery. Angioplasty (opening the constricted area with a balloon) may also be performed.[3]
Other complications
Hydrocephalus (obstruction of the flow of cerebrospinal fluid) may complicate SAH in both the short- and long term. It is detected on CT scanning, on which there is enlargement of the lateral ventricles. If the level of consciousness is decreased, drainage of the excess fluid is performed by therapeutic lumbar puncture, extraventricular drain (a temporary device inserted into the one of the ventricles) or occasionally a permanent shunt.[1][3] Relief of hydrocephalus can lead to an enormous improvement in a person's condition.[5] Fluctuations in blood pressure and electrolyte disturbances, as well as pneumonia and cardiac decompensation occur in about half the hospitalized persons with SAH and may worsen prognosis.[1] Seizures occur during the hospital stay in about a third of cases.[3] Many believe that patients might benefit from prevention with antiepileptic drugs.[3] Although this is widely practiced,[38] it is controversial and not based on good evidence.[39][40] In some studies, use of these drugs was associated with a worse prognosis; this might be because they actually cause harm, or because they are used more often in persons with a poorer prognosis.[41][42] There is a possibility of a gastric hemorrhage due to stress ulcers.[43]
Prognosis
Early morbidity and mortality
SAH is often associated with a poor outcome.[2] The death rate (mortality) for SAH is between 40 and 50%,[14] but trends for survival are improving.[1] Of those who survive hospitalization, more than a quarter have significant restrictions in their lifestyle, and less than a fifth have no residual symptoms whatsoever.[28] Delay in diagnosis of minor SAH (mistaking the sudden headache for migraine) contributes to poor outcome.[15] Factors found on admission that are associated with poorer outcome include poorer neurological grade; systolic hypertension; a previous diagnosis of heart attack or SAH; liver disease; more blood and larger aneurysm on the initial CT scan; location of an aneurysm in the posterior circulation; and higher age.[41] Factors that carry a worse prognosis during the hospital stay include occurrence of delayed ischemia resulting from vasospasm, development of intracerebral hematoma or intraventricular hemorrhage (bleeding into the ventricles of the brain) and presence of fever on the eighth day of admission.[41]
So-called "angiogram-negative subarachnoid hemorrhage", SAH that does not show an aneurysm with four-vessel angiography, carries a better prognosis than SAH with aneurysm; however, it is still associated with a risk of ischemia, rebleeding and hydrocephalus.[11] Perimesencephalic SAH (bleeding around the mesencephalon in the brain), however, has a very low rate of rebleeding or delayed ischemia, and the prognosis of this subtype is excellent.[44]
The prognosis of head trauma is thought to be influenced in part by the location and amount of subarachnoid bleeding.[12] It is difficult to isolate the effects of SAH from those of other aspects of traumatic brain injury; it is unknown whether the presence of subarachnoid blood actually worsens the prognosis or whether it is merely a sign that a significant trauma has occurred.[12] People with moderate and severe traumatic brain injury who have SAH when admitted to a hospital have as much as twice the risk of dying as those who do not.[12] They also have a higher risk of severe disability and persistent vegetative state, and traumatic SAH has been correlated with other markers of poor outcome such as post traumatic epilepsy, hydrocephalus, and longer stays in the intensive care unit.[12] However, more than 90% of people with traumatic subarachnoid bleeding and a Glasgow Coma Score over 12 have a good outcome.[12]
There is also modest evidence that genetic factors influence the prognosis in SAH. For example, having two copies of ApoE4 (a variant of the gene encoding apolipoprotein E that also plays a role in Alzheimer's disease) seems to increase risk for delayed ischemia and a worse outcome.[45] The occurrence of hyperglycemia (high blood sugars) after an episode of SAH confers a higher risk of poor outcome.[46]
Long-term outcomes
Neurocognitive symptoms, such as fatigue, mood disturbances, and other related symptoms are common sequelae. Even in those who have made good neurological recovery, anxiety, depression, posttraumatic stress disorder and cognitive impairment are common; 46% of people who have suffered a subarachnoid hemorrhage have cognitive impairment that affects their quality of life.[3] Over 60% report frequent headaches.[47] Aneurysmal subarachnoid hemorrhage may lead to damage of the hypothalamus and the pituitary gland, two areas of the brain that play a central role in hormonal regulation and production. More than a quarter of people with a previous SAH may develop hypopituitarism (deficiencies in one or more of the hypothalamic-pituitary hormones such as growth hormone, luteinizing hormone or follicle-stimulating hormone).[48]
Epidemiology

According to a review of 51 studies from 21 countries, the average incidence of subarachnoid hemorrhage is 9.1 per 100,000 annually. Studies from Japan and Finland show higher rates in those countries (22.7 and 19.7, respectively), for reasons that are not entirely understood. South and Central America, in contrast, have a rate of 4.2 per 100,000 on average.[49]
Although the group of people at risk for SAH is younger than the population usually affected by stroke,[2] the risk still increases with age. Young people are much much less likely than middle-aged people (risk ratio 0.1, or 10%) to suffer a subarachnoid hemorrhage.[49] The risk continues to rise with age and is 60% higher in the very elderly (over 85) than in those between 45 and 55.[49] Risk of SAH is about 25% higher in women over 55 compared to men the same age, probably reflecting the hormonal changes that result from the menopause, such as a decrease in estrogen levels.[49]
Genetics may play a role in a person's disposition to SAH; risk is increased three- to fivefold in first-degree relatives of people who have suffered a subarachnoid hemorrhage.[4] However, lifestyle factors are more important in determining overall risk.[2] These risk factors are smoking, hypertension (high blood pressure) and excessive alcohol intake.[14] Having smoked in the past confers a doubled risk of SAH compared to those who have never smoked.[2] Some protection of uncertain significance is conferred by Caucasian ethnicity, hormone replacement therapy, diabetes mellitus and higher than normal levels of cholesterol.[2] Approximately 4% of aneurysmal bleeds occur after sexual intercourse and 10% of people with SAH are bending over or lifting heavy objects at the onset of their symptoms.[5]
Overall, about 1% of all people have one or more cerebral aneurysms. Most of these, however, are small and unlikely to rupture.[25]
History
While the clinical picture of subarachnoid hemorrhage may have been recognized by Hippocrates, the existence of cerebral aneurysms and the fact that they could rupture was not established until the 18th century.[50] The associated symptoms were described in more detail in 1886 by Edinburgh physician Dr Byrom Bramwell.[51] In 1924, London neurologist Sir Dr Charles P. Symonds (1890–1978) gave a complete account of all major symptoms of subarachnoid hemorrhage, and he coined the term "spontaneous subarachnoid hemorrhage".[50][52][53] Symonds also described the use of lumbar puncture and xanthochromia in diagnosis.[54]
The first surgical intervention was performed by Mr Norman Dott, who was a pupil of Dr Harvey Cushing then working in Edinburgh. He introduced the wrapping of aneurysms in the 1930s, and was an early pioneer in the use of angiograms.[53] American neurosurgeon Dr Walter Dandy, working in Baltimore, was the first to introduce clips in 1938.[26] Microsurgery was applied to aneurysm treatment in 1972 in order to further improve outcomes.[55] The 1980s saw the introduction of triple H therapy[36] as a treatment for delayed ischemia due to vasospasm, and trials with nimodipine[34][56] in an attempt to prevent this complication. In 1983, the Russian neurosurgeon Zubkov and colleagues reported the first use of transluminal balloon angioplasty for vasospasm after aneurysmal SAH.[57][58] The Italian neurosurgeon Dr Guido Guiglielmi introduced his endovascular coil treatment in 1991.[27][59]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 van Gijn J, Kerr RS, Rinkel GJ (2007). "Subarachnoid haemorrhage". Lancet 369 (9558): 306–18. doi:10.1016/S0140-6736(07)60153-6. PMID 17258671.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Feigin VL, Rinkel GJ, Lawes CM, et al. (2005). "Risk factors for subarachnoid hemorrhage: an updated systematic review of epidemiological studies". Stroke 36 (12): 2773–80. doi:10.1161/01.STR.0000190838.02954.e8. PMID 16282541. http://stroke.ahajournals.org/cgi/content/full/36/12/2773.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Suarez JI, Tarr RW, Selman WR (January 2006). "Aneurysmal subarachnoid hemorrhage". New England Journal of Medicine 354 (4): 387–96. doi:10.1056/NEJMra052732. PMID 16436770.
- ↑ 4.0 4.1 4.2 Longmore, Murray; Ian Wilkinson, Tom Turmezei, Chee Kay Cheung (2007). Oxford Handbook of Clinical Medicine, 7th edition. Oxford University Press. pp. 841. ISBN 0-19-856837-1.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 Ramrakha, Punit; Kevin Moore (2007). Oxford Handbook of Acute Medicine, 2nd edition. Oxford University Press. pp. 466–470. ISBN 0-19-852072-6.
- ↑ 6.0 6.1 6.2 6.3 Warrell, David A; Timothy M. Cox, et al. (2003). Oxford Textbook of Medicine, Fourth Edition, Volume 3. Oxford. pp. 1032–1034. ISBN 0-19-857013-9.
- ↑ McCarron MO, Alberts MJ, McCarron P (2004). "A systematic review of Terson's syndrome: Frequency and prognosis after subarachnoid haemorrhage". Journal of Neurology, Neurosurgery, and Psychiatry 75 (3): 491–3. doi:10.1136/jnnp.2003.016816. PMID 14966173. PMC 1738971. http://jnnp.bmj.com/cgi/content/full/75/3/491.
- ↑ Allman, Keith G.; Iain H. Wilson (2006). Oxford Handbook of Anaesthesia, 2nd edition. Oxford University Press. pp. 408–409. ISBN 0198566090.
- ↑ Banki NM, Kopelnik A, Dae MW, et al. (2005). "Acute neurocardiogenic injury after subarachnoid hemorrhage". Circulation 112 (21): 3314–9. doi:10.1161/CIRCULATIONAHA.105.558239. PMID 16286583. http://circ.ahajournals.org/cgi/content/full/112/21/3314.
- ↑ Servadei F, Murray GD, Teasdale GM, et al. (February 2002). "Traumatic subarachnoid hemorrhage: demographic and clinical study of 750 patients from the European brain injury consortium survey of head injuries". Neurosurgery 50 (2): 261–7; discussion 267–9. doi:10.1097/00006123-200202000-00006. PMID 11844260.
- ↑ 11.0 11.1 11.2 11.3 Rinkel GJ, van Gijn J, Wijdicks EF (1 September 1993). "Subarachnoid hemorrhage without detectable aneurysm. A review of the causes" (PDF). Stroke 24 (9): 1403–9. PMID 8362440. http://stroke.ahajournals.org/cgi/reprint/24/9/1403.
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 12.6 12.7 Armin SS, Colohan AR, Zhang JH (June 2006). "Traumatic subarachnoid hemorrhage: Our current understanding and its evolution over the past half century". Neurological Research 28 (4): 445–52. doi:10.1179/016164106X115053. PMID 16759448.
- ↑ 13.0 13.1 13.2 Cruickshank A, Auld P, Beetham R, et al. (May 2008). "Revised national guidelines for analysis of cerebrospinal fluid for bilirubin in suspected subarachnoid haemorrhage". Annals of Clinical Biochemistry 45 (Pt 3): 238–44. doi:10.1258/acb.2008.007257. PMID 18482910. http://acb.rsmjournals.com/cgi/content/full/45/3/238.
- ↑ 14.0 14.1 14.2 Teunissen LL, Rinkel GJ, Algra A, van Gijn J (1 March 1996). "Risk factors for subarachnoid hemorrhage: a systematic review". Stroke 27 (3): 544–9. PMID 8610327. http://stroke.ahajournals.org/cgi/content/full/27/3/544.
- ↑ 15.0 15.1 Kowalski RG, Claassen J, Kreiter KT, et al. (February 2004). "Initial misdiagnosis and outcome after subarachnoid hemorrhage". Journal of the American Medical Association 291 (7): 866–9. doi:10.1001/jama.291.7.866. PMID 14970066. http://jama.ama-assn.org/cgi/content/full/291/7/866.
- ↑ Nguyen H, Zaroff JG (November 2009). "Neurogenic stunned myocardium". Curr Neurol Neurosci Rep 9 (6): 486–91. PMID 19818236.
- ↑ Rosen D, Macdonald R (2005). "Subarachnoid hemorrhage grading scales: A systematic review". Neurocritical Care 2 (2): 110–8. doi:10.1385/NCC:2:2:110. PMID 16159052.
- ↑ Hunt W, Hess R (1968). "Surgical risk as related to time of intervention in the repair of intracranial aneurysms". Journal of Neurosurgery 28 (1): 14–20. doi:10.3171/jns.1968.28.1.0014. PMID 5635959.
- ↑ Fisher C, Kistler J, Davis J (1980). "Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning". Neurosurgery 6 (1): 1–9. doi:10.1097/00006123-198001000-00001. PMID 7354892.
- ↑ Claassen J, Bernardini GL, Kreiter K, et al. (September 2001). "Effect of cisternal and ventricular blood on risk of delayed cerebral ischemia after subarachnoid hemorrhage: the Fisher scale revisited". Stroke 32 (9): 2012–20. doi:10.1161/hs0901.095677. PMID 11546890. http://stroke.ahajournals.org/cgi/content/full/32/9/2012.
- ↑ Teasdale G, Drake C, Hunt W, Kassell N, Sano K, Pertuiset B, De Villiers J (1988). "A universal subarachnoid hemorrhage scale: Report of a committee of the World Federation of Neurosurgical Societies". Journal of Neurology, Neurosurgery, and Psychiatry 51 (11): 1457. doi:10.1136/jnnp.51.11.1457. PMID 3236024.
- ↑ 22.0 22.1 Ogilvy CS, Carter BS (May 1998). "A proposed comprehensive grading system to predict outcome for surgical management of intracranial aneurysms". Neurosurgery 42 (5): 959–68; discussion 968–70. doi:10.1097/00006123-199805000-00001. PMID 9588539.
- ↑ 23.0 23.1 White PM, Wardlaw JM (December 2003). "Unruptured intracranial aneurysms". Journal of Neuroradiology 30 (5): 336–50. PMID 14752379. http://www.em-consulte.com/article/126528.
- ↑ Gibbs GF, Huston J, Qian Q, et al. (May 2004). "Follow-up of intracranial aneurysms in autosomal-dominant polycystic kidney disease". Kidney International 65 (5): 1621–7. doi:10.1111/j.1523-1755.2004.00572.x. PMID 15086900.
- ↑ 25.0 25.1 International Study of Unruptured Intracranial Aneurysms Investigators (December 1998). "Unruptured intracranial aneurysms—risk of rupture and risks of surgical intervention". New England Journal of Medicine 339 (24): 1725–33. doi:10.1056/NEJM199812103392401. PMID 9867550. http://content.nejm.org/cgi/content/full/339/24/1725.
- ↑ 26.0 26.1 Dandy WE (1938). "Intracranial aneurysm of the internal carotid artery: Cured by operation". Annals of Surgery 107 (5): 654–9. doi:10.1097/00000658-193805000-00003. PMID 17857170.
- ↑ 27.0 27.1 Guglielmi G, Viñuela F, Dion J, Duckwiler G (1991). "Electrothrombosis of saccular aneurysms via endovascular approach. Part 2: Preliminary clinical experience". Journal of Neurosurgery 75 (1): 8–14. doi:10.3171/jns.1991.75.1.0008. PMID 2045924.
- ↑ 28.0 28.1 28.2 28.3 Molyneux AJ, Kerr RS, Yu LM, et al. (2005). "International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: A randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion". Lancet 366 (9488): 809–17. doi:10.1016/S0140-6736(05)67214-5. PMID 16139655.
- ↑ van der Schaaf I, Algra A, Wermer M, et al. (2005). "Endovascular coiling versus neurosurgical clipping for patients with aneurysmal subarachnoid haemorrhage". Cochrane Database of Systematic Reviews (Online) (4): CD003085. doi:10.1002/14651858.CD003085.pub2. PMID 16235314. http://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD003085/frame.html.
- ↑ Campi A, Ramzi N, Molyneux AJ, et al. (2007). "Retreatment of ruptured cerebral aneurysms in patients randomized by coiling or clipping in the International Subarachnoid Aneurysm Trial (ISAT)". Stroke 38 (5): 1538–44. doi:10.1161/STROKEAHA.106.466987. PMID 17395870. http://stroke.ahajournals.org/cgi/content/full/38/5/1538.
- ↑ Piotin M, Spelle L, Mounayer C, et al. (2007). "Intracranial aneurysms: Treatment with bare platinum coils—aneurysm packing, complex coils, and angiographic recurrence". Radiology 243 (2): 500–8. doi:10.1148/radiol.2431060006. PMID 17293572. http://radiology.rsnajnls.org/cgi/content/full/243/2/500.
- ↑ Raymond J, Guilbert F, Weill A, et al. (2003). "Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils". Stroke 34 (6): 1398–403. doi:10.1161/01.STR.0000073841.88563.E9. PMID 12775880. http://stroke.ahajournals.org/cgi/content/full/34/6/1398.
- ↑ 33.0 33.1 Dorhout Mees S, Rinkel G, Feigin V, et al. (2007). "Calcium antagonists for aneurysmal subarachnoid haemorrhage". Cochrane Database of Systematic Reviews (Online) (3): CD000277. doi:10.1002/14651858.CD000277.pub3. PMID 17636626.
- ↑ 34.0 34.1 Allen GS, Ahn HS, Preziosi TJ, et al. (1983). "Cerebral arterial spasm: A controlled trial of nimodipine in patients with subarachnoid hemorrhage". New England Journal of Medicine 308 (11): 619–24. PMID 6338383.
- ↑ Vergouwen MD, Vermeulen M, Roos YB (December 2006). "Effect of nimodipine on outcome in patients with traumatic subarachnoid haemorrhage: A systematic review". Lancet Neurology 5 (12): 1029–32. doi:10.1016/S1474-4422(06)70582-8. PMID 17110283.
- ↑ 36.0 36.1 Kassell NF, Peerless SJ, Durward QJ, Beck DW, Drake CG, Adams HP (September 1982). "Treatment of ischemic deficits from vasospasm with intravascular volume expansion and induced arterial hypertension". Neurosurgery 11 (3): 337–43. doi:10.1097/00006123-198209000-00001. PMID 7133349.
- ↑ Sen J, Belli A, Albon H, Morgan L, Petzold A, Kitchen N (October 2003). "Triple-H therapy in the management of aneurysmal subarachnoid haemorrhage". Lancet Neurology 2 (10): 614–21. doi:10.1016/S1474-4422(03)00531-3. PMID 14505583.
- ↑ Rosengart AJ, Huo JD, Tolentino J, et al. (August 2007). "Outcome in patients with subarachnoid hemorrhage treated with antiepileptic drugs". Journal of Neurosurgery 107 (2): 253–60. doi:10.3171/JNS-07/08/0253. PMID 17695377.
- ↑ Naval NS, Stevens RD, Mirski MA, Bhardwaj A (February 2006). "Controversies in the management of aneurysmal subarachnoid hemorrhage". Critical Care Medicine 34 (2): 511–24. doi:10.1097/01.CCM.0000198331.45998.85. PMID 16424735.
- ↑ Liu KC, Bhardwaj A (2007). "Use of prophylactic anticonvulsants in neurologic critical care: a critical appraisal". Neurocritical Care 7 (2): 175–84. doi:10.1007/s12028-007-0061-5. PMID 17763834.
- ↑ 41.0 41.1 41.2 Rosengart AJ, Schultheiss KE, Tolentino J, Macdonald RL (August 2007). "Prognostic factors for outcome in patients with aneurysmal subarachnoid hemorrhage". Stroke 38 (8): 2315–21. doi:10.1161/STROKEAHA.107.484360. PMID 17569871. http://stroke.ahajournals.org/cgi/content/full/38/8/2315.
- ↑ Naidech AM, Kreiter KT, Janjua N, et al. (March 2005). "Phenytoin exposure is associated with functional and cognitive disability after subarachnoid hemorrhage". Stroke 36 (3): 583–7. doi:10.1161/01.STR.0000141936.36596.1e. PMID 15662039. http://stroke.ahajournals.org/cgi/content/full/36/3/583.
- ↑ Lindsay, Kenneth W; Ian Bone, Robin Callander (1993). Neurology and Neurosurgery Illustrated. United States: Churchill Livingstone. ISBN 0-443-04345-0.
- ↑ Greebe P, Rinkel GJ (April 2007). "Life expectancy after perimesencephalic subarachnoid hemorrhage". Stroke 38 (4): 1222–4. doi:10.1161/01.STR.0000260093.49693.7a. PMID 17332451. http://stroke.ahajournals.org/cgi/content/full/38/4/1222.
- ↑ Lanterna LA, Ruigrok Y, Alexander S, et al. (August 2007). "Meta-analysis of APOE genotype and subarachnoid hemorrhage: clinical outcome and delayed ischemia". Neurology 69 (8): 766–75. doi:10.1212/01.wnl.0000267640.03300.6b. PMID 17709709.
- ↑ Kruyt ND, Biessels GJ, de Haan RJ, et al. (June 2009). "Hyperglycemia and clinical outcome in aneurysmal subarachnoid hemorrhage: a meta-analysis". Stroke 40 (6): e424–30. doi:10.1161/STROKEAHA.108.529974. PMID 19390078.
- ↑ Powell J, Kitchen N, Heslin J, Greenwood R (June 2002). "Psychosocial outcomes at three and nine months after good neurological recovery from aneurysmal subarachnoid haemorrhage: Predictors and prognosis". Journal of Neurology, Neurosurgery, and Psychiatry 72 (6): 772–81. doi:10.1136/jnnp.72.6.772. PMID 12023423. PMC 1737916. http://jnnp.bmj.com/cgi/content/full/72/6/772.
- ↑ Schneider HJ, Kreitschmann-Andermahr I, Ghigo E, Stalla GK, Agha A (September 2007). "Hypothalamopituitary dysfunction following traumatic brain injury and aneurysmal subarachnoid hemorrhage: a systematic review". Journal of the American Medical Association 298 (12): 1429–38. doi:10.1001/jama.298.12.1429. PMID 17895459. http://jama.ama-assn.org/cgi/content/full/298/12/1429.
- ↑ 49.0 49.1 49.2 49.3 49.4 de Rooij NK, Linn FH, van der Plas JA, Algra A, Rinkel GJ (December 2007). "Incidence of subarachnoid haemorrhage: A systematic review with emphasis on region, age, gender and time trends". Journal of Neurology, Neurosurgery, and Psychiatry 78 (12): 1365–72. doi:10.1136/jnnp.2007.117655. PMID 17470467.
- ↑ 50.0 50.1 Longstreth WT, Koepsell TD, Yerby MS, van Belle G (1985). "Risk factors for subarachnoid hemorrhage" (PDF). Stroke 16 (3): 377–85. PMID 3890278. http://stroke.ahajournals.org/cgi/reprint/16/3/377.pdf.
- ↑ Bramwell B (1886). "Spontaneous meningeal haemorrhage". Edinburgh Medical Journal 32: 101.
- ↑ Symonds CP (1924). "Spontaneous subarachnoid hemorrhage". Quarterly Journal of Medicine 18: 93–122.
- ↑ 53.0 53.1 Todd NV, Howie JE, Miller JD (June 1990). "Norman Dott's contribution to aneurysm surgery". Journal of Neurology, Neurosurgery, and Psychiatry 53 (6): 455–8. doi:10.1136/jnnp.53.6.455. PMID 2199609.
- ↑ Symonds CP (1924). "Spontaneous sub-arachnoid hæmorrhage". Proceedings of the Royal Society of Medicine 17 (Neurol Sect): 39–52. PMID 19983808.
- ↑ Krayenbühl HA, Yaşargil MG, Flamm ES, Tew JM (December 1972). "Microsurgical treatment of intracranial saccular aneurysms". Journal of Neurosurgery 37 (6): 678–86. doi:10.3171/jns.1972.37.6.0678. PMID 4654697.
- ↑ Pickard JD, Murray GD, Illingworth R, et al. (March 1989). "Effect of oral nimodipine on cerebral infarction and outcome after subarachnoid haemorrhage: British aneurysm nimodipine trial". BMJ (Clinical research ed.) 298 (6674): 636–42. doi:10.1136/bmj.298.6674.636. PMID 2496789.
- ↑ Zubkov IuN, Nikiforov BM, Shustin VA (Sep-Oct 1983). "1st attempt at dilating spastic cerebral arteries in the acute stage of rupture of arterial aneurysms". Zh Vopr Neirokhir Im N N Burdenko 5 (5): 17–23. PMID 6228084.
- ↑ Zubkov YN, Nikiforov BM, Shustin VA (Sep-Oct 1984). "Balloon catheter technique for dilatation of constricted cerebral arteries after aneurysmal SAH". Acta Neurochir (Wien) 70 (1-2): 65–79. doi:10.1007/BF01406044. PMID 6234754.
- ↑ Strother CM (1 May 2001). "Historical perspective. Electrothrombosis of saccular aneurysms via endovascular approach: part 1 and part 2". AJNR. American Journal of Neuroradiology 22 (5): 1010–2. PMID 11337350. http://www.ajnr.org/cgi/content/full/22/5/1011.
External links
- Neuroland SAH page
|
|||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||